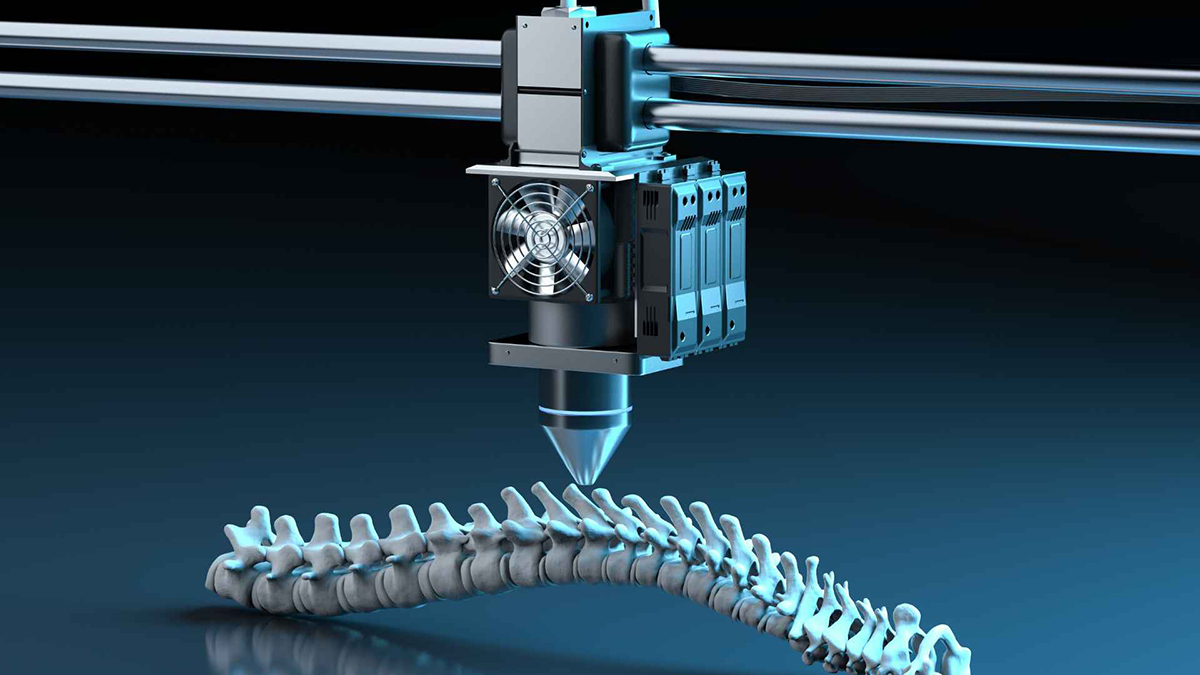
Providence Medical Technology, Inc., a medical device innovator focused on improving surgical outcomes for high-risk spine surgery patients, today announced a new publication in the Journal of Clinical Neuroscience. Dr. Michael M. Haglund and colleagues authored the publication on the long-term outcomes of patients undergoing tissue-sparing Posterior Cervical Fusion (PCF) to revise a 1-level pseudarthrosis following a failed Anterior Cervical Discectomy and Fusion (ACDF).
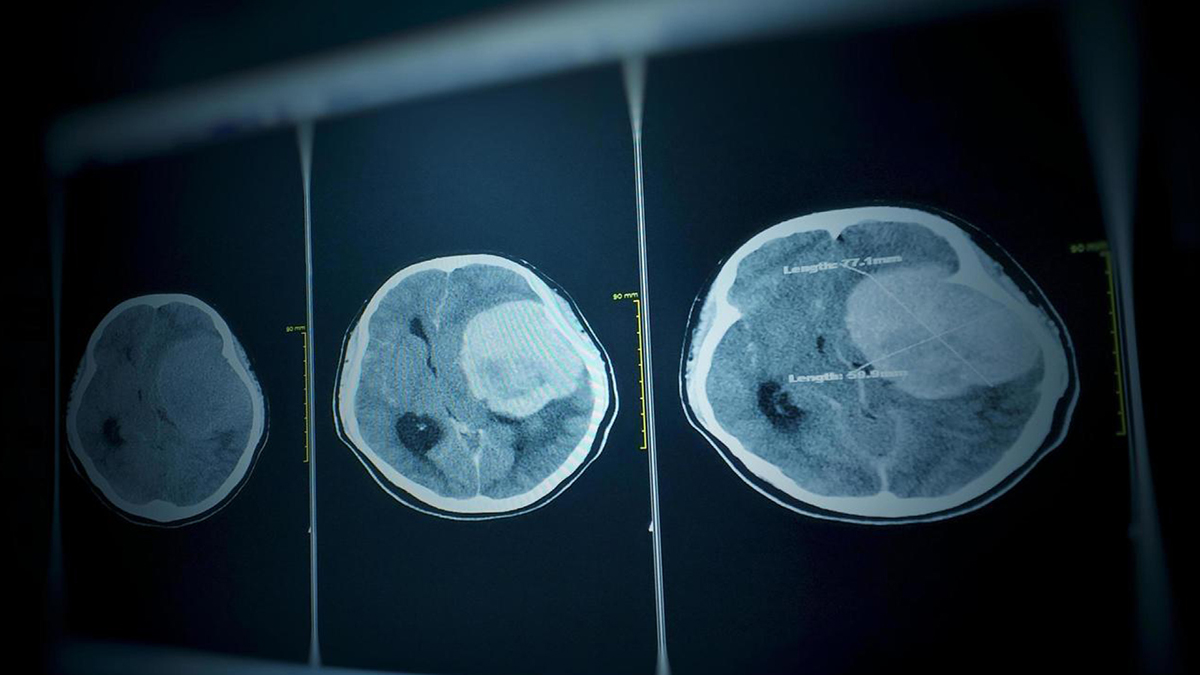
There are over 300,000 cervical fusion procedures performed each year, with over 40% involving patients with some form of risk factors for nonunion. While safe and effective for most patients, a common complication is pseudarthrosis, a failure of the bones to heal and fuse after surgery. Risk factors that contribute to pseudarthrosis include multi-level disease, poor bone quality, smoking, diabetes, and insufficient immobilization. When pseudarthrosis occurs, patients can experience severe pain and neurological issues, which often necessitate another surgical intervention. This second “revision” surgery can be more complex and carry increased risks and complications.
The Journal of Clinical Neuroscience publication presents long-term data on forty-five patients enrolled from six sites across the United States who had a failed cervical fusion surgery (ACDF) and were subsequently revised with a tissue-sparing posterior cervical fusion using Providence Medical Technology’s CORUS™ Spinal System and CAVUX® FFS.
Key findings from the study include:
- High Success Rate: Surgeons observed complete fusion (bone healing) in 91% of cases. An independent core imaging lab observed motion less than two degrees in 93% of cases and verified continuous bridging bone across the treated joints in 80% of patients.
- High Satisfaction Rate: 74% of subjects reported satisfaction with their revision surgery outcomes.
- Reduced Surgery Time, Blood Loss, & Hospital Stay: Tissue-sparing PCF had a median procedure time of 49 minutes, an estimated blood loss of just 10 cc, and a median hospital stay of one day.
- No Hospital Re-admission or Subsequent Surgical Interventions: None of the patients in the study went on to an additional surgery or re-admission following their tissue-sparing revision procedure with a median follow-up time of over three years.
CAVUX® FFS is a unique surgical implant constructed of a CAVUX Cervical Cage and an ALLY® Bone Screw. Two FFS devices are implanted bilaterally through the back of the neck and span the facet joints to provide immobilization and stabilization as an adjunct to posterior cervical fusion. CAVUX FFS is “indicated for patients requiring a revision for an anterior pseudarthrosis at one level, from C3 to C7, with autogenous and/or allogenic bone graft.” CAVUX FFS is implanted using the company’s flagship CORUS™ Spinal System, which enables a surgeon to perform a tissue-sparing posterior cervical fusion before placing implants.
“Tissue-sparing posterior cervical fusion with CORUS™ Spinal System and CAVUX® FFS has become my preferred approach to treating patients after a failed anterior fusion,” said Dr. Michael M. Haglund, Endowed Professor of Neurosurgery and Orthopaedic Surgery at Duke University and lead author of the publication. “I am pleased to publish this new evidence demonstrating positive results in this difficult to treat patient population.”
“Failed spine surgery is a huge problem for everyone involved,” Providence CEO and Co-founder Jeff Smith noted. “High-risk spinal fusion patients suffer nonunion rates much higher than most people realize and often require revision surgery. We believe this is not acceptable and are driven to prevent these failures for all patients. Our tissue-sparing posterior fusion technology is a great option to treat these patients, as is well demonstrated in this study. We also believe the best way to fix surgical failures among high-risk spinal fusion patients is to prevent them from happening in the first place. We look forward to sharing our FUSE study data in the coming months for this application. I am so thankful for the support of all of our research partners for both of these studies. They are truly dedicated to solving this unmet clinical need for high-risk patients.”
Providence Medical Technology devices have been used to treat over 20,000 patients and are currently available in over 2,500 hospitals in the United States.
About Providence Medical Technology, Inc.
Providence Medical Technology, Inc. is a privately held medical device company focused on innovative and tissue-sparing surgical solutions for cervical spine surgery. Its purpose is to improve clinical outcomes for high-risk patients and prevent surgical failures of the cervical spine. Its mission is to establish Circumferential Cervical Fusion (CCF) as the standard of care for high-risk patients. The Company has pioneered a proprietary approach to posterior cervical and lumbar fusion and has developed surgical instrumentation and implants that address the unmet clinical need of and offer unique benefits to the $2 billion worldwide cervical spine market.
The Providence family of products includes the CORUS™ Spinal System, CAVUX® intervertebral implants, and ALLY® bone and facet screws. All implants and instruments are sterile-packaged and single-use to maximize perioperative efficiency and ensure consistent quality and performance.